An Urgent and Intentional Matter: Supporting Minority Mental Health
Here at the New England MHTTC, we are acknowledging Minority Mental Health Month through our continued commitment to intentionally address racial equity disparities this month and year-round.
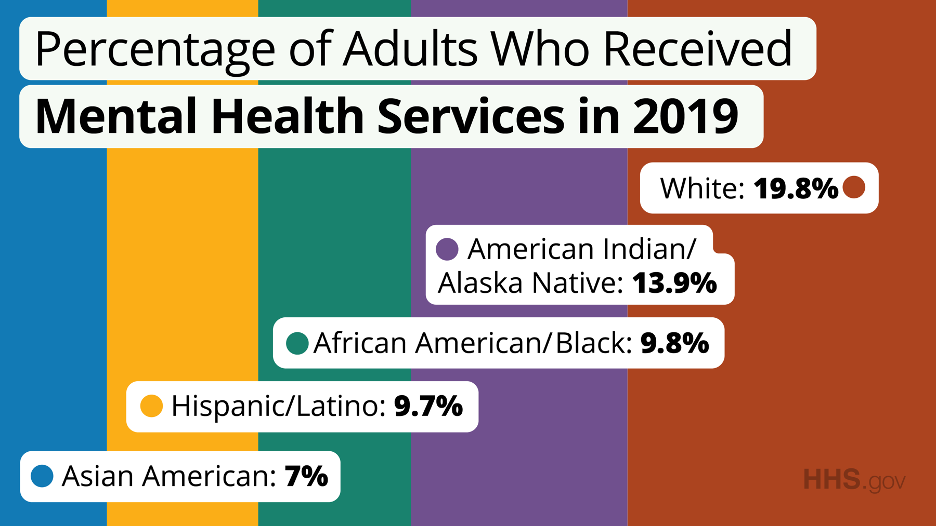
While approximately 1 in 5 Americans experience mental illness, people who are members of minority communities are more likely to experience risk factors that can cause mental health challenges. When seeking care and support, Black, Latinx, Indigenous, Asian, and other People of Color face structural racism, discrimination, and stigma in health care systems and from health care providers as well as challenges accessing culturally appropriate care. According to the U.S. Department of Health and Human Services, 19.8% of white adults received mental health services in 2019 compared to 13.9% of American Indian/Alaska Native people, 9.8% of African American/Black people, 9.7% of Hispanic/Latino people, and 7% of Asian American people.
Since 2020, the COVID-19 pandemic has disproportionately affected Black, Indigenous, and People of Color and made it even harder to access care. In addition, the consequences of mental illness among people who are members of minority communities can persist. For example, according to the American Pyschiatric Association, depression among people who are Black and Hispanic is likely to be more persistent, and American Indians/Alaskan Natives report higher rates of post-traumatic stress disorder and alcohol dependence than any other racial or ethnic group.
We hope you and your colleagues will attend these upcoming events and use the following resources year-round to support mental health and resiliency for people who are members of minority communities.
Resources
Providing Culturally Responsive Care and Addressing Cross-Cultural Barriers in Early Psychosis
Why is Culturally Responsive Care important, and what do we really mean? Many factors impact disparities, including social and economic conditions that influence the diagnosis a patient receives and the prevalence or extent to which individuals develop mental illness. A wide body of research points toward adverse circumstances, systemic factors, and elements innate to our social fabric as increasing adverse life events and mental illness.
Culturally Responsive Care is a system that celebrates individual differences and incorporates humility, intentionality, an anti-oppressive framework, and full acknowledgement for unique experiences into all aspects of care. Culturally Responsive Care helps identify structural barriers that cultural diversity faces in the mental healthcare system by addressing the social fabric that influences diagnoses by honoring the person’s own cultural explanatory model and letting it inform diagnostic decisions.
What follows Culturally Responsive Care is cultural competency—a concept that
acknowledges how personal and structural racism and other forms of oppression
may lead to the denial of treatment resources and services, which lead to significantly worse mental health outcomes, mistrust, and fear of treatment especially for marginalized communities that experience continued systemic discrimination.
Racial and ethnic communities struggle, in part, from social determinants of mental illness such as discrimination and social exclusion and in the ways our current mental
healthcare system interprets the presentation of symptoms. For instance, Director of the Chinese Mental Health Program at the University of Massachusetts, Dr. Xiaoduo Fan, emphasizes in Understanding and Treating Psychosis and Other Mental Illnesses in the Context of Asian Cultures and Anti-Asian Racism that in Buddhism, being an intermediary between ancestors and immediate family is considered a praiseworthy identity. However, the clinical manifestation of this identity is more often interpreted as a sign of risk for psychosis. A culturally responsive approach has the potential to create a working differential between racial/ethnic communities experiencing mental illness due to discrimination, social exclusion, and systematic oppression, and racial/ethnic communities being misdiagnosed by culturally deaf clinical models of symptom interpretation.
To learn more, access New England MHTTC’s online series for clinicians to provide culturally responsive care and address cross-cultural barriers in early psychosis from the early psychosis initiative at Beth Israel Deaconess Medical Center/Harvard Medical School. This series follows the governing principles of shared decision-making and cultural competence to interpret and facilitate recovery. We explore the unique cultural impact on an individual’s openness to care, perceptions of care, and treatment adherence, including types of acceptable treatment and treatment duration.
Learn More