Home > MIC Stories: Traumatic Brain Injury and Mental Health - Intensive Workshops
MIC Stories (MHTTCs Implementing Change) feature technical assistance projects that had a significant impact on practice.
Throughout rural and frontier communities, traumatic brain injury (TBI) is routinely identified as a common presenting problem with limited resources to support treatment, and patients with TBI often carry additional diagnoses that increase complexity when accessing treatment. In addition, health and behavioral health care providers have identified needing more training and information on TBI. This topic was identified as a high priority and area for collaboration through the Mountain Plains MHTTC’s Needs Assessment and in discussion with SAMHSA Regional Administrator Dr. Charles Smith.
Through collaboration with Dr. Smith’s office, the Mountain Plains MHTTC leveraged a connection with the National Association of State Head Injury Administrators (NASHIA) to provide a comprehensive workshop series on evidence-based practices for supporting persons with TBI and co-occurring mental health disorders.
All sessions were hosted virtually due to the COVID-19 pandemic. This series was focused on serving participants in HHS Region 8, but participants attended from across the United States
Due to the intensive nature of each of the workshops, participants completed a brief application for review by NASHIA and Mountain Plains MHTTC staff, and each workshop was limited to 20 attendees. Staff selected attendees based on their work and personal experience, and familiarity with the culture of each community. The Mountain Plains MHTTC project coordinator also worked closely with SAMHSA Regional Administrator Dr. Charles Smith and NASHIA staff to identify and develop lists of regional and national communities of interest. Building on these lists, the Mountain Plains MHTTC staff conducted targeted outreach efforts via email and social media to engage specific community members (i.e., veterans’ groups for the veteran intensive workshop, educators for the K-12 intensive workshop) before each intensive workshop.
A total of 255 people from approximately 15 organizations participated across the sessions. Participants included social workers, counselors, psychologists, nurses, researchers, educators, addiction professionals, recovery specialists, and peer professionals. Organizations represented a variety of settings, including community-based organizations, mental health clinics, substance use disorder treatment programs and prevention programs, hospitals, elementary and secondary education settings, criminal justice, primary care physicians, group homes, and FQHC.
From July to October 2020, the Mountain Plains MHTTC hosted a virtual series, Traumatic Brain Injury and Mental Health: Intensive Workshops, featuring experienced trainers from NASHIA. We began with an introductory session providing foundational knowledge to allow attendees to develop a foundational understanding of TBI and how it impacts individuals. Participants in this introductory session were encouraged to then enroll in intensive workshops to develop deeper understanding of providing treatment for specific populations with co-occurring TBI and behavioral health disorders (Veterans, school-age youth, primary care providers, and those with co-occurring substance use disorders). The intensive workshops included 60 minutes of special topic instruction and 30 minutes of Q&A, allowing participants to explore challenges and barriers to providing care while receiving information from experts. The series also included a panel discussion hosted by state head injury administrators from across HHS Region 8 that connected attendees with state specific resources to decrease barriers to care and foster connections and relationships between administrators and service providers.
As with most mental health treatment areas, the lack of insurance coverage and prioritized funding for evidence-based treatment continues to be one of the largest barriers to care for patients and providers. Additionally, TBI can be difficult to diagnose because many of its symptoms are similar to other mental health conditions, especially co-occurring substance use disorders.
Providers who attended this series reported a better understanding of key TBI information, including symptomology and treatment. They also reported increased connection to training information and state level resources following training sessions centered on state-specific resources.
Of participants who completed a post-event survey:
This training series leveraged existing relationships in the various TBI communities located throughout Region 8. It also highlighted the effectiveness of the collaboration between the National Association of State Head Injury Administrators (NASHIA) and the SAMSHA HHS Region 8 offices in addressing this topic. Given the challenges identified by trainers, training attendees, and national advocacy groups, increasing provider awareness and understanding regarding the treatment of traumatic brain injury by continuing to provide training will be critical to providing high-quality, evidence-based care for people living with a TBI in Region 8.
Workshop recordings, slide decks, and additional materials from the series can all be accessed here: Traumatic Brain Injury and Mental Health: Intensive Workshops

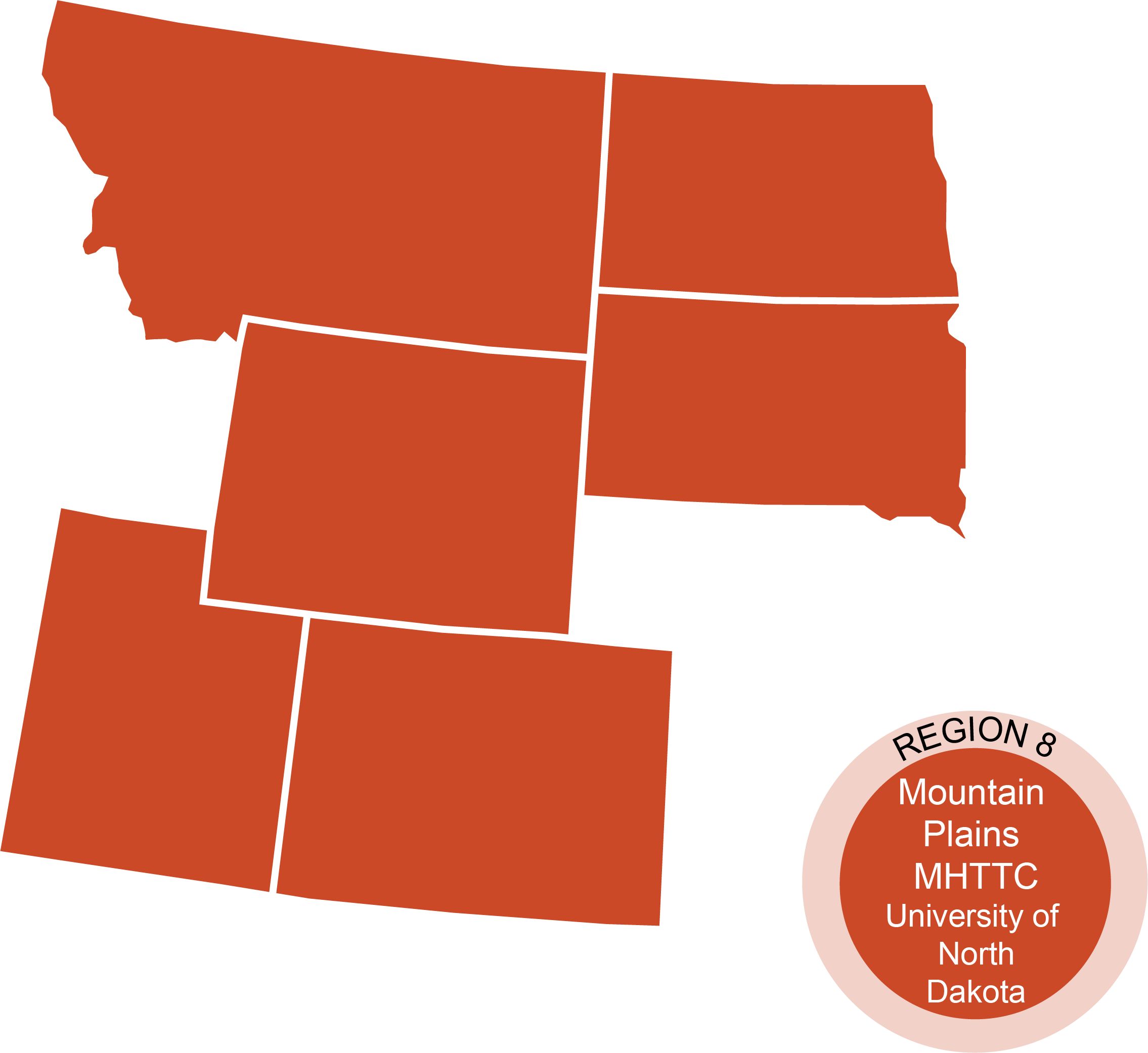
The Mountain Plains Mental Health Technology Transfer Center (MHTTC) is one of the 12 centers that make up the larger MHTTC Network. The primary focus of the Center is to provide training, resources, and technical assistance to individuals serving persons with mental health disorders. Particular attention is given to serving providers with limited access to service delivery systems to include a focus on rural and agricultural communities. By providing free, innovative, and accessible learning opportunities on research-based practices in mental health services, we seek to help you better serve your communities, staff, and patients. The Mountain Plains MHTTC serves the states of Colorado, Montana, North Dakota, South Dakota, Utah, and Wyoming.
Goals of the Mountain Plains MHTTC