Home > Integrated Care Webinar Series 2021
What do we understand about interventions to reduce racial and ethnic disparities in access to mental health care? View this webinar recording for a look at integrated care and policy interventions that support equity in mental health care delivery. This presentation illustrated an historical perspective on mental health policy and race-based inequities, and how to reduce these disparities. Clinicians will learn deeply why they need to understand why and how systemic racism influences decisions to seek care or avoid care.
Pamela Collins, MD, MPH, is Professor of Psychiatry and Behavioral Sciences and Professor of Global Health at the University of Washington, where she is Executive Director of I-TECH and director of the UW Global Mental Health Program, a joint effort of the Department of Psychiatry & Behavioral Sciences and the Department of Global Health. She is a psychiatrist and mixed methods researcher with 25 years of experience in global public health and global mental health research, education, training and capacity-building, and science policy leadership. Prior to her current role she directed the Office for Research on Disparities & Global Mental Health and the Office of Rural Mental Health Research at the National Institute of Mental Health (NIMH) (USA). She has served the field in diverse leadership roles, most recently as a commissioner for the Lancet Commission on Global Mental Health and Sustainable Development, a leader of the Grand Challenges in Global Mental Health initiative, co-lead of the NIMH-PEPFAR initiative on mental health and HIV, a member of the World Economic Forum’s Agenda Council on Mental Health, and the director of the RISING SUN initiative on suicide prevention in Arctic Indigenous communities. Her research has focused on social stigma related to mental illness and its relationship to HIV risk among women of color with severe mental illness; the intersections of mental health with HIV prevention, care, and treatment; and the mental health needs of diverse groups in the US, Latin America and Sub-Saharan Africa. She is currently the Principal Investigator of EQUIP Nairobi: a pilot implementation of Trauma-Focused CBT in Nairobi, Kenya, part of a more comprehensive effort to meet the mental health needs of children and adolescents in Nairobi.
Dr. Phillip Hawley from the Yakima Valley Farm Workers Clinic outlines the foundations of the primary care behavioral health (PCBH) model of integration and discusses a variety of clinical applications. He explains why meeting patients where they are and working within the primary care system provides holistic and quality patient care. Dr. Hawley also provides statistics and case examples highlighting how this approach covers gaps in our healthcare system and works towards true population health strategies. This training's learning objectives are:
Dr. Phillip Hawley is the Primary Care Behavioral Health Director for the Yakima Valley Farm Workers Clinic (YVFWC). Phillip is a Licensed Clinical Psychologist and has worked in primary care for the past 6 years. Phillip manages the Primary Care Behavioral Health program, consisting of 17 BHCs across Washington and Oregon who provide behavioral health service within the PCBH model of integration. Phillip’s role as director includes: Site visits and ongoing support of BHC within the organization, reporting for internal and external stakeholders, supervision for the BHC post-doctoral residents, hiring/ onboarding and training of newly hired BHCs, coordination with regional healthcare and behavioral health organizations through sub-committees and workgroups, direct patient care through same day consultation, and providing in-service trainings to assess mental health concerns to staff and the community. Phillip is focused on assisting in complete health care for patients. Phillip and his wife reside in Naches, WA.
Providers from the Lummi Tribal Health Center describe and discuss the unique challenges to providing psychiatric care in a coordinated and collaborative way to a tribal community during the coronavirus pandemic. This training's learning objectives are:
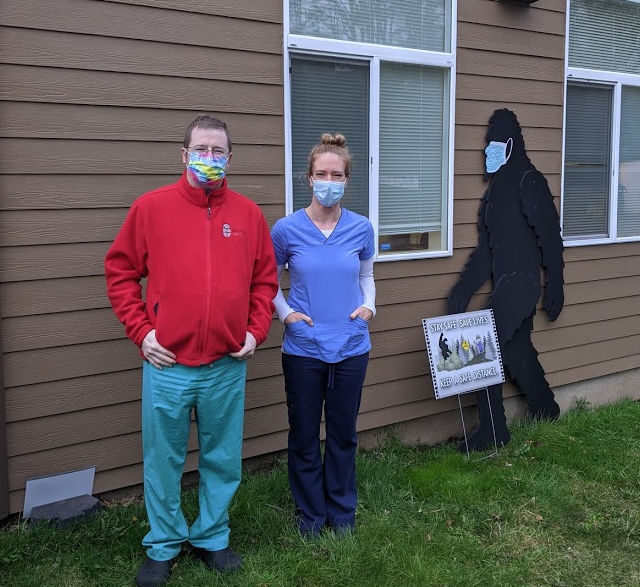 George ‘Bud’ Vana, MD, is a Triple Boarder – having taken three board exams as a general pediatrician, adult psychiatrist and child psychiatrist – practicing at the Lummi Tribal Health Center in Bellingham, Washington. He and his psychiatric team are integrated and collocated (before coronavirus) in the medical clinic, substance abuse program, pediatrics department, school-based health clinic and behavioral health department. He finished his BA and MA at Harvard University in Near Eastern Languages and Civilization. He completed medical school at the University of Vermont and completed residency training at Brown University in Providence, Rhode Island. He completed his outpatient psychiatry training at the Providence Rhode Island Veterans Administration. He has worked to develop a telehealth infrastructure at the Lummi Tribal Health Center as well as a child psychiatry consultation service for other tribal health clinics. His other professional interests include family-based psychiatry, acceptance and commitment therapy, treatment of co-occurring disorders, treatment of developmental disabilities and integrated medical and behavioral healthcare. Outside of work he enjoys canoeing, hiking and curling (as in the Olympic ice sport) with his family in Bellingham.
George ‘Bud’ Vana, MD, is a Triple Boarder – having taken three board exams as a general pediatrician, adult psychiatrist and child psychiatrist – practicing at the Lummi Tribal Health Center in Bellingham, Washington. He and his psychiatric team are integrated and collocated (before coronavirus) in the medical clinic, substance abuse program, pediatrics department, school-based health clinic and behavioral health department. He finished his BA and MA at Harvard University in Near Eastern Languages and Civilization. He completed medical school at the University of Vermont and completed residency training at Brown University in Providence, Rhode Island. He completed his outpatient psychiatry training at the Providence Rhode Island Veterans Administration. He has worked to develop a telehealth infrastructure at the Lummi Tribal Health Center as well as a child psychiatry consultation service for other tribal health clinics. His other professional interests include family-based psychiatry, acceptance and commitment therapy, treatment of co-occurring disorders, treatment of developmental disabilities and integrated medical and behavioral healthcare. Outside of work he enjoys canoeing, hiking and curling (as in the Olympic ice sport) with his family in Bellingham.
Born and raised in the Pacific Northwest, Jessica McLendon, CMA, first received her Bachelor of Arts in Anthropology and Global Studies at Pacific Lutheran University. After moving to Bellingham, she started working in the non-profit field for Big Brothers Big Sisters of Northwest Washington and later, at Northwest Youth Services, a housing provider for homeless youth. In 2017 she completed her certification in Medical Assisting and started working at Lummi Tribal Health Clinic in 2018. Jessica is passionate about witnessing peoples’ stories and connecting individuals to the appropriate resources to help them achieve their goals.
Cedric Robertson serves as a Peer Recovery Coach at the Lummi Tribal Health Center.